First, Do No Harm
Appealing to nature doesn't cut it.
UPDATED: January 12, 2026
Welcome to the Healthy Living Is Good Medicine Newsletter, presenting timely, science-based, original articles covering a wide range of preventive medicine and public health topics, along with critical commentaries on the politics and economics of the American healthcare system.
The Appeal to Nature Fallacy
Unscrupulous practitioners and salespersons frequently exploit the flawed argument that something is inherently good because it is “natural,” or bad because it is “unnatural.” That claim ignores the many natural things that are harmful, and the many artificial things that are beneficial.
This logical fallacy bypasses rationality and scientific evidence by emotionally appealing to a common bias against the unfamiliar. Just because something is “natural” doesn’t mean that it is good for our health. For example, the Death Cap (Amanita phalloides) and Destroying Angel (Amanita virosa) wild mushrooms are 100 percent natural and 100 percent organic, but even a tiny bite contains enough alpha amantin to kill you, and it’s a particularly nasty way to die. More than 20 poisonings and one death related to eating wild mushrooms have been reported in California alone.
Raw milk and raw vegetables of all kinds can present a much higher risk for food-borne illnesses than their pasteurized or cooked versions. For example, the fecal contamination of USDA certified organic frozen strawberries has resulted in outbreaks of hepatitis A.
Practitioners of so-called “alternative medicine” often push supplements of no proven value and dubious purity and potency, with claims that because they are “natural” they are better for health and far less harmful than the synthetic chemicals found in pharmaceuticals. Consumers need to be aware that this is a sales pitch, not science.
Medicine’s Guiding Principle
The universal precept of the medical profession is, “First, do no harm.” The phrase is attributed to the 4th century BCE Greek physician Hippocrates, considered the father of modern medicine, and is found in his work, “Of the Epidemics.” This ethical cornerstone of medicine was later popularized by the 17th century English physician, Thomas Sydenham, as primum non nocere.
This is the foundational principle of medical ethics. We must always weigh the potential harms of a preventive intervention, medical treatment, or surgical procedure against its potential benefits, and assess the risks as they apply to individual patients. This has to be done subjectively, because risks and benefits use different metrics and cannot be compared quantitatively.
Clinical trials are also held to that standard. Exposing participants to known risks is highly unethical. That hasn’t stopped antivax HHS Secretary RFK Jr. from calling for RCTs (randomized controlled trials) on vaccines that already have an extensive record of safety and efficacy. His claim that the childhood vaccine schedule has never been tested in RCTs using saline placebo controls is a deceptive half-truth that ignores both what constitutes a scientifically valid placebo and the ethical requirements.
Now, think about all the harm that’s done when needed medical services are denied by insurers, life-saving prescription medications are unaffordable, and preventive healthcare is inaccessible. These are just some of the blatant harms done when ruthless capitalism runs amok in the healthcare system.
The avoidance of harms needs to figure prominently in the decision-making processes for both doctors and their patients, keeping in mind that there are situations where doing nothing can be harmful. The reality is that there are always risks and benefits to every medical intervention, and there are also risks and benefits to every non-intervention. Physicians need to walk a fine line between the two.
That guiding principle needs to be taken into account by political leaders and government policy makers. We are currently witnessing the wholesale destruction of America’s world-leading national public health system. Eviscerating the U.S. Centers for Disease Control and Prevention (CDC) for political gain, while implementing misguided health policies, will inevitably produce disastrous results for the public, both at home and abroad. Politicians and their appointees in government are displaying an alarming degree of incompetence, something that has never been seen before.
It grieves me to say that under the current Trump administration and his appointees we can no longer trust the once revered national institutions of science and medicine. RFK Jr. has arbitrarily cut a number of medically recommended childhood vaccinations, endorsed quack treatments, and changed dietary guidelines to favor meat and cheese, all without solid scientific evidence. CMS administrator Mehmet Oz encouraged people to drink alcohol, echoing the talking points of the alcohol industry. This kind of bureaucratic insanity has greatly undermined the public’s trust in both science and the federal government itself.
The public will now need to rely upon non-governmental sources for their health information. Let consumers beware; charlatans abound. Don’t do your own “online research” or you are likely to fall prey to bad advice. Your own M.D. or D.O. is best qualified to give you personalized professional advice. Even then, if they are not up to speed on the latest research, ask for a referral to a specialist. Even then, seeking a second opinion may be warranted.
It can also be helpful to have a patient advocate on your side if you need help navigating the healthcare system or finding reliable online information. The challenge will always involve separating accurate health information from the misinformation, but there are a number of pointers that can help you in recognizing the “red flags” and locating high-quality information sources.
There are also harmful systemic problems. America’s profit-driven healthcare system is inherently harmful, because it prioritizes corporate wealth over patient health. The basic formula for this kind of capitalistic system’s success involves extracting the most money possible from patients, while exploiting the good intentions of their healthcare providers. This has resulted in widespread harms, such as denying patients necessary medical care and inflicting moral injuries upon medical providers:
Weighing the Evidence
If the totality of the evidence currently available is insufficient to reach a sound therapeutic decision, a physician might want to adopt a watch-and-wait approach, known as applying “the tincture of time.” In other words, when in doubt, do nothing!
This precautionary principle emphasizes preventing harm in the face of uncertain risks or the absence of conclusive scientific evidence regarding efficacy and safety. It advocates for erring on the side of caution in order to protect the public’s health and minimize potential harms to the patient.
The problem is that patients want solutions, and they want them now. At the same time, doctors want to be helpful and offer their patients something, rather than send them home empty-handed and tell them to come back in a few days if they aren’t feeling better. The expectations are amplified by clever pharmaceutical industry marketing strategies that imply there’s a cure for every ailment.
The standards of medical practice argue against hastily employing treatments that come with risks of serious adverse effects. Additional laboratory tests and imaging studies may be necessary to narrow down the differential diagnosis. In most situations, time is on the side of the clinician, but in a true medical or surgical emergency, delaying a risky treatment could mean flirting with disaster.
Decision-making becomes even more complicated when the studies of a specific treatment's outcomes have produced contradictory results. One would still seek to minimize risks, but there would be a lot more uncertainty about how to best go about doing that. Fortunately, when it comes to weighing potential benefits against potential harms, vaccines in general are overwhelmingly beneficial. The pseudoscientific, alarmist arguments of anti-vaccine conspiracy theorists can be summarily dismissed.
Doctors want to avoid iatrogenic illnesses and other medical complications caused by their actions. Medical errors are, unfortunately, not uncommon, and can be a major cause of injury and death, according to some studies. It is important for patients to recognize the significant challenges that can accompany standard medical and surgical care, and understand the risks versus benefits ratios that they may be facing:
Risk Tolerance
Some people are adrenaline junkies and love taking risks and living dangerously. That's not me. Although I've enjoyed participating in a few high-risk sports, I was aware of their inherent dangers, analyzed their risks, and did everything I could to minimize them. Thanks to a little extra luck, I'm still here to tell the tale. The flip side to my adventurousness is that in addition to keeping up-to-date with my COVID-19 vaccinations, I still wear an N95 mask in indoor public spaces, which I consider to be a minimal inconvenience in exchange for mitigating the risks.
It is a sad fact that our for-profit healthcare system provides financial incentives for risky medical and surgical procedures. The general rule seems to be that more aggressive interventions receive higher insurance reimbursements. For example, the overuse of coronary artery stents puts hundreds of thousands of patients in harm’s way, when there are less invasive (and less lucrative) alternatives. Private health insurance typically pays more than $20,000 per stent procedure.
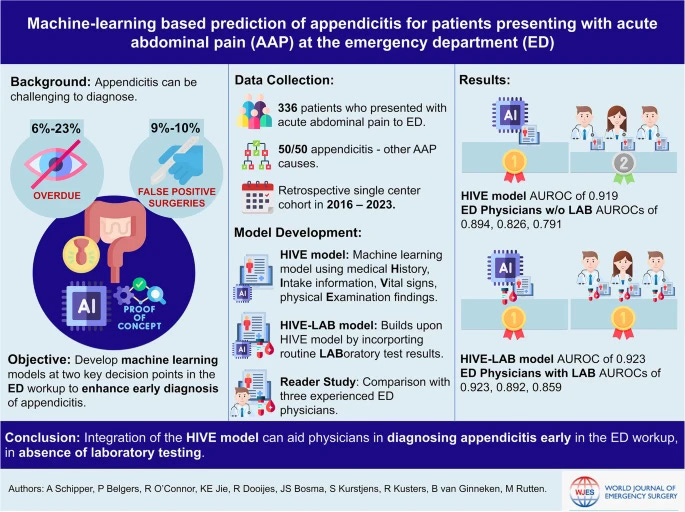
An indelible lesson from one of my surgical rotations was that in a certain percentage of patients diagnosed with acute appendicitis, a surgeon will remove an appendix that is totally normal. There will be another percentage in which an appendix has already burst. An appendectomy carries less risk than an infected appendix spilling bacteria into the abdominal cavity, so erring on side of caution means operating unnecessarily in a certain number of cases.
A competent and ethical surgeon will strive for a 10-20 percent negative appendectomy rate. Hopefully, that's the surgeon you would get if you show up in the emergency department with right lower quadrant pain. Rates that fall above that range indicate that a surgeon is too eager to cut, and rates that are lower suggest that they are putting patients at greater risk for peritonitis and septic shock.
Questioning Proposed Treatments
The road to patient harm is paved with click-bait headlines based upon provisional conclusions from observational studies. When they are later refuted by negative clinical trials, they will receive scant attention by the media. People don’t show much in interest in what doesn’t work, but they sure get excited about something new that seems to.
Added to that, there’s a barrage of direct-to-consumer drug advertising (“Ask your doctor…”) on TV and in other media. The risks and adverse effects are presented, but you’ll miss them if you’re not paying close attention. There’s an amazing difference in what you’ll learn from a TV drug ad if you close your eyes and just focus on the audio.
The doctor you’re supposed to ask if the drug is right for you has their own set of obstacles to overcome. Patient pressure to try something they saw on TV, unfamiliarity with the scientific literature, personal biases, and the time constraints of office visits can become a formula for therapeutic missteps. That’s why patients need to educate themselves about their health challenges and play an active role in any decision-making.
The list of ineffective or harmful medical therapies, along with myriad bogus treatments pushed by quacks, is quite long, yet more are continually being added. Please be skeptical of non-prescription treatments extolled by your Facebook friends, TikTok influencers, or suggested by your chiropractor, naturopath, acupuncturist, or massage therapist. When there’s a choice, give a nod to prescription medications that have a long record of efficacy and safety, especially when there are less expensive generic versions available.
Disregard patient testimonials, and those from sell-out doctors. Instead, seek the opinions of bonafide medical experts in their respective fields. Then, consider getting a second opinion from another physician who is equally qualified. It can be quite unsettling when two competent specialists, presented with the same patient data, can differ in their opinions about the best course of treatment. It is therefore up to patients to weigh the pros and cons of each, and decide what seems best for them.
Burden of Proof
Let's not confuse legal terminology with medical and scientific jargon. Technically speaking, "proof" is a mathematical concept. Legal proof for something that's alleged to be true, is different, but is clearly defined by the law. Science offers conditional validation, rather than absolute proof. We can't prove that an hypothesis is true, but we can subject it to experiments that attempt to falsify it.
Probable cause is a legal standard that means a reasonable person would believe that a crime has been, is being, or is about to be committed. It is an absolute requirement under the Fourth Amendment to the U.S. Constitution that must be met before law enforcement officers can search a location, obtain a search warrant, or make an arrest.
Preponderance of the evidence is the legal burden of proof in most civil cases. It means that each element of a claim must be found more likely to be true than not. Science does not accept such a lax standard, but sometimes medical judgments will have to rely upon it, when that's the best evidence available.
Beyond a reasonable doubt is a guiding principle of the U.S. criminal justice system. Prosecutions must begin with a presumption of innocence. The prosecution must prove someone's guilt by offering enough evidence to erase a reasonable person's doubts about it. An American legal doctrine, proposed in 1769 by William Blackstone, states that it is better for 10 guilty people to go free than to wrongfully convict an innocent person. This moral rationale for protecting the innocent dates back to Roman times.
The law does not require absolute certainty to reach a verdict. Conclusions in science are never based upon complete certainty either. Science only provides the probable degree to which an evidence-based conclusion could be accurate. Those conclusions are always subject to invalidation by new data. Study results are typically expressed in terms of the confidence that an outcome isn't due to chance alone.
In medical research, the best evidence for causal relationships between an intervention or exposure and the outcome is derived from randomized, controlled trials (RCTs). Typically, participants in an RCT are randomly selected to be either in a treatment group or a control group that gets a placebo. When the study is double-blinded, neither the researchers nor the subjects will know who got the placebo until the study is concluded.
An RCT's data is then analyzed, discussed, and interpreted. A reputable study will discuss its possible sources of error and disclose the researchers' potential conflicts of interest. Its conclusions will be couched in a specific degree of certainty, which is never 100 percent. The authors will typically present numerical ranges around average values, known as the 95 percent confidence interval. The narrower the range, the more confidence one can have in the study's results not being due to chance.
For the conclusions from an RCT to be more convincing, the study will need to be independently replicated and reach similar conclusions. In practice, this rarely occurs because research grants usually fund original studies. In any case, most medical studies are not RCTs. Rather, they are observational studies, either looking back in time, or waiting to see what the future outcome of an intervention or exposure will be for a particular population. Such studies are weakened by their inability to control confounding variables.
Preventive Medicine and Risk Management
When it comes to preventive medicine, it is difficult to find convincing scientific evidence supporting some lifestyle interventions. The health impacts of treatments, interventions, and environmental exposures may be cumulative, or take a long time to appear in human subjects. Since observational studies will never be able to establish causal relationships, physicians must often make patient recommendations based upon a preponderance of the best currently available scientific evidence.
Let's not ignore the fact that much of the so-called "research" published in "junk journals" does not adhere to strict scientific criteria. Most doctors don't have enough time to keep up with the latest research, and it may be necessary to take a deep dive into the medical literature to separate the wheat from the chaff. Here’s a primer on how to make sense of a study:
That could be impractical for busy practicing physicians who are not also scientists. Consequently, doctors must do the best they can. while facing a certain amount of uncertainty. When in doubt, it's generally better for physicians to err on the side of caution. Taking a more conservative (risk minimizing) approach when making medical decisions requires sound clinical judgment and a consideration of the individual patient's needs. However, this isn’t always appropriate in emergency care settings, where unnecessary interventions could harm patients, strain resources, and drive up costs.
When a doctor's good-faith advice later turns out to be incorrect, as long as it has not critically delayed appropriate treatment, it should not have produced any significant harms. However, despite our best intentions, that's not always the case. We certainly aren't able to predict someone's future, and we can't insist that they heed our best yet fallible advice.
We can only inform our patients about what we know regarding the potential risks and benefits of various courses of action. If statistical probabilities are available, we can share them, while pointing out that statistics apply only to populations, not individuals. Once fully informed, it is then up to the patient to make decisions about their healthcare. Hopefully, good information provided by their doctors will lead to good decisions.
However, some patients may not want to make those decisions. Many patients will be swayed by their emotions. How can anyone still reeling from a cancer diagnosis rationally decide to undergo a difficult course of post-operative chemotherapy that carries a risk of permanent neurological or cardiac damage? When there's only a five percent chance that their type of cancer will recur following surgery without subsequent treatment, how will that impact their decision? Sadly, I have had a few patients who declined chemo because they thought the odds were greatly in their favor. They gambled, and as it turned out, they were among the five-percenters.
Moral of the story: If you want to increase your chance of survival following a life-threatening cancer diagnosis, do everything you can to push the odds of a cure toward 100 percent, even if it means risking serious side-effects from the "standard-of-care" treatments. Case in point: Diagnosed with pancreatic cancer, Apple Computer's co-founder, Steve Jobs, “trusted his intuition” rather than his doctor's advice, and sought alternative treatments. That allowed his cancer to advance until it became incurably fatal. I hope his doctor told him that delaying appropriate medical treatment would be crazy.
Chicken Soup for Colds
When it comes to treating symptoms of the common cold, there may not be anything that’s much better than chicken soup. According to one study, its slight anti-inflammatory effect could result in symptom relief. Even if only evokes a placebo effect, recommending homemade chicken soup for a common cold is far less harmful than prescribing antibiotics that can adversely impact the gut microbiome.
Many of the products found on drugstore shelves were grandfathered in by the FDA more than 50 years ago. Over-the-counter (OTC) drug manufacturers have been pushing a plethora of products using the same old ingredients, without having to prove their efficacy. New requirements for OTC drugs are much more stringent. In September, 2023, the FDA’s advisors concluded that the common nasal decongestant, phenylephrine, was ineffective, but the FDA cannot force its removal from the market.
One of the biggest mistakes that doctors can make is giving in to patient pressure and prescribing antibiotics for upper respiratory tract infections caused by a virus. Doctors who don't do what their patients want or expect risk receiving low ratings on doctor-scoring websites. The inappropriate prescribing of antibiotics contributes to the emergence of microbes that are resistant to multiple drugs. As a result, infectious organisms that are difficult or impossible to treat now present a global health threat.
The science regarding the contamination of foods with industrial and agricultural chemicals, and the long-term health risks that might pose, clearly isn't perfect, but the information we do have is what we have to go on. Can eating lots of pesticide-laced strawberries be harmful? The answer is a definite “maybe.” But who wants to be the guinea pig in that experiment? A recent review has highlighted the potential consequences of pesticide exposure in disrupting the gut microbiome.
Making Health Recommendations
I’m not an infallible expert. However, I do try to communicate the best health information that I can gather from what appear to be credble resources, while navigating my way through a morass of online misinformation. The problem I face is that in the time I have available to produce an article, I can’t do a deep dive into the materials and methods used in all the research upon which I rely for my conclusions and suggestions.
There are only so many hours of the day in which to be productive, and it would be impractical for me to independently determine the validity of all the researchers’ results upon which I base my “in general” recommendations. I just give it my best shot, in the limited time that I have available. Remember, I’m not making my living by writing articles or prescribing for patients. Hopefully, my peers will let me know if I’ve missed the mark, and I will then make the necessary corrections in an update.
Even when scientists have done everything that they can to draw evidence-based conclusions from their research, they can still be wrong. Science continually progresses, with self-correction as part of the process. If I can’t tolerate the risk being wrong when I write an article, should I simply remain silent? Obviously, if I have something to say, I’ll say it.
It might be preferable to make a Type 1 Error (false positive conclusion) than a Type 2 Error (false negative conclusion), but both error types should be avoided. Wasting resources trying to protect oneself from non-existent dangers also comes with the risk of developing maladaptive behaviors.
Contrast those consequences with wrongly concluding that something is benign, and not taking adequate precautions. In certain situations, tending toward Type 1 Errors could be advantageous, provided the cost of missing a real threat is significantly higher than the cost of a false alarm.
Individuals vary greatly in their risk tolerance or aversion, as well as in their ability to afford and employ potential mitigation measures. People will need to evaluate the information I’ve provided and decide for themselves. I hope that whatever you decide, you'll favor healthier choices, and remember…
First, do no harm! Humanity would surely be a lot better off if everyone made that principle an everyday practice.
This Post may be updated at any time. Please check back here again to find the latest information on this subject.
Find more articles about Healthy Living in my Post Archive.
Please share my Website Link with others via your social media accounts.
You can help your friends and followers become healthier by suggesting that they subscribe to this Newsletter. You may receive access to premium features as a thank-you for making referrals:
If you find this Newsletter of value, and want to lend your support, please make a donation that will help it reach many more people: