Trusting Your Gut
Making friends with our microbiome.
UPDATED: January 11, 2026
Welcome to the Healthy Living Is Good Medicine Newsletter, presenting timely, science-based, original articles covering a wide range of preventive medicine and public health topics, along with critical commentaries on the politics and economics of the American healthcare system.
The more I learn about all our microbiomes and their co-evolution with humans, and the more I discover about how the health of our microbiomes affects our own health in many different ways, the more attention and care I'm willing to invest in treating my unseen companions kindly. From what I can tell, having a harmonious, mutually advantageous relationship with our beneficial resident microbes is good medicine.
Our Unseen Companions
The human gastrointestinal (GI) tract is populated by a community of bacteria, fungi, archaea, and viruses. Although these microscopic organisms are living out of sight, they continue to make headlines with further evidence indicating that a diverse and well-balanced population of microbes in our gut is crucial for our health.
There are an estimated 100 trillion organisms living inside our GI tract, rivaling the number of cells in our bodies. Although found in large numbers in the mouth and small intestine, most of them reside in our large intestine. They are collectively known as the gut microbiome.
Most of our internal passengers are either harmless or beneficial, but a Helicobacter pylori infection of the stomach can cause ulcers, and sometimes cancer. A dangerous Clostridioides difficile superinfection of the bowel can occur when antibiotics alter the normal bacterial flora, allowing C. diff to proliferate and release toxins that cause intestinal damage.
In addition to the dysbiosis caused by antibiotics, other medications that impact the composition of the intestinal microbiome include antivirals, antifungals, anthelmintics, proton pump inhibitors, nonsteroidal anti-inflammatory drugs, laxatives, oral antidiabetics, antidepressants, antipsychotics, statins, chemotherapeutics, and immunosuppressants. According to a 2020 study, of 41 classes of medications, 19 were associated with changes in the gut microbiome.
Human anatomy, physiology, and behavior have all been shaped through the process of natural selection, in which the members of our species that were best adapted to survive in their environment were able to pass their genetic traits and accumulated knowledge on to their descendants. Evolution takes place over hundreds of thousands of years. Along with our human body and mind, our microbiome has co-evolved.
For most of that time, our hominid ancestors lived in a very unsanitary world. It has been suggested that a lack of diversity in our microbiome today could potentially contribute to the higher incidence of metabolic and inflammatory diseases that have become so common in the developed world.
There's a growing body of evidence suggesting that childhood exposure to microorganisms in dirt can decrease their risk of developing asthma. Studies have consistently shown that children who grow up on farms, particularly those with livestock, have a lower risk of developing asthma and allergies. Our skin microbiome also plays a crucial role in maintaining skin health. Bathing too often can disrupt that population’s balance, potentially leading to problems such as eczema and acne.
Research on the gut microbiome indicates that early life microbial exposures also plays an important role in the development of the immune system. Establishing a favorable gut microbiome appears essential for proper immune function and regulation. Microbial colonization of the gut begins at birth and continues throughout early childhood. This early colonization is critical for the immune system being able to distinguish between harmless substances and organisms, and those that are harmful.
The industrialization of our food supply and modern food processing practices have resulted in the limited ingestion of microbes, with the exception of fermented foods that contain live bacterial cultures, and foods contaminated with the pathogenic organisms that cause food poisoning.
In Gut We Trust
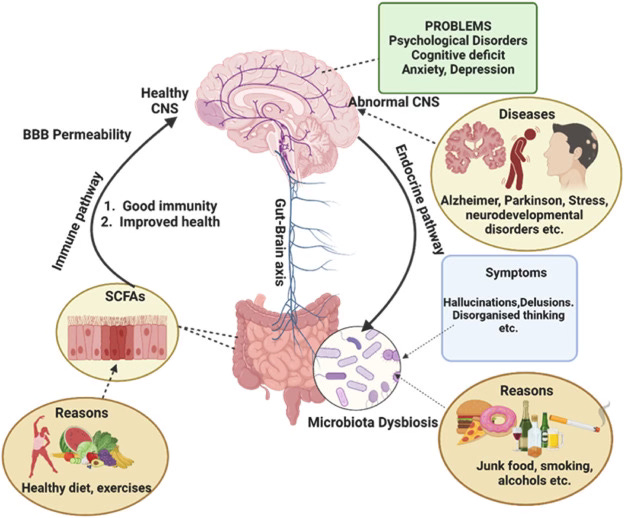
Recent studies have uncovered relationships between the composition of our gut microbiome and the functioning of our liver, kidneys, and muscles. An even more fascinating connection is known as the gut-brain axis. It suggests a relationship with our microbiome that influences our moods and behaviors. Other studies have suggested that the gut microbiome can play a role in mental health. An interesting article explores how the influence of diet upon the microbiome can impact the brain. I like to think of “gut farming” as optimizing our gastrointestinal microbiome through lifestyle interventions.
New research suggests that our cravings for specific dietary components originate from signals sent from the gut. For example, the metabolites produced by gut microbes such as Bacteroides vulgatus may influence a person's sweet tooth via GLP-1 and the FGF21 hormone. One study showed that people with a genetic deficiency in FGF21 production are predisposed to eat more sweet foods. Chemical communication between our resident intestinal microbes and our body’s cells seems to play a role in hunger, satiety, sugar-cravings, and the development of obesity.
Research has established the existence of two-way communication between the gut and the brain. Other studies have shown a relationship between the microbiome and the immune system. Research also establishes the role of the microbiome in mental health. A 2021 review suggests that the amino acid glutamine can positively affect gut health by supporting the microbiome, improving gut mucosal wall integrity, and by modulating inflammation. In addition, there may be a positive effect on neuropsychiatric conditions via the gut-brain axis.
People differ in the kinds of resident microbes living in and on their bodies. The trillions of microorganisms in the human gastrointestinal tract influence digestion and overall health. However, microbiome testing comes with a number of caveats. Let the consumer beware!
Populations of harmful gut microbes have been associated with increased risks for illnesses such as type 2 diabetes, liver disease, cancer, autoimmune diseases, and cardiovascular disease. As important as it now appears, there are still many unknowns regarding the exact mechanisms involved in the microbiome’s impact upon health and illness.
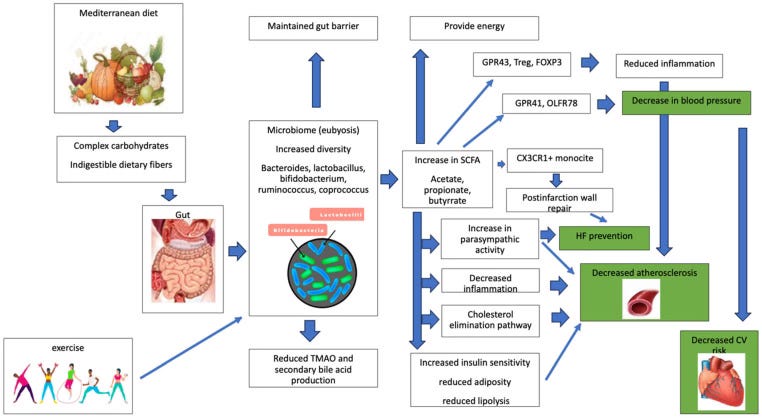
In a recent study, researchers identified several species of bacteria whose populations had an influence upon cholesterol, triglycerides, and blood glucose levels. Higher populations of Oscillibacter sp. were strongly associated with lower levels of LDL (“bad”) cholesterol. The organism’s impact on cholesterol levels appears due to the presence of bacterial enzymes that break down cholesterol in the intestine. Another study found that the gut microbiome has a potential role in increasing the risk of diabetes by those who consume large quantities of sugar-sweetened beverages.
Consequently, we are well advised to treat our intestinal microbiome kindly, if we want it to support our health. The mysteries associated with our internal passengers are being probed by scientists, and evidence continues to accumulate that alterations in the composition of intestinal populations are associated with increased risks for illnesses.
Some studies suggest that disruptions in the gut microbiome may contribute to the development of neurological disorders, such as Parkinson's disease, Alzheimer's disease, and autism. Other studies point to the importance of gut health during early life for proper brain development and function.
The Role of Diet
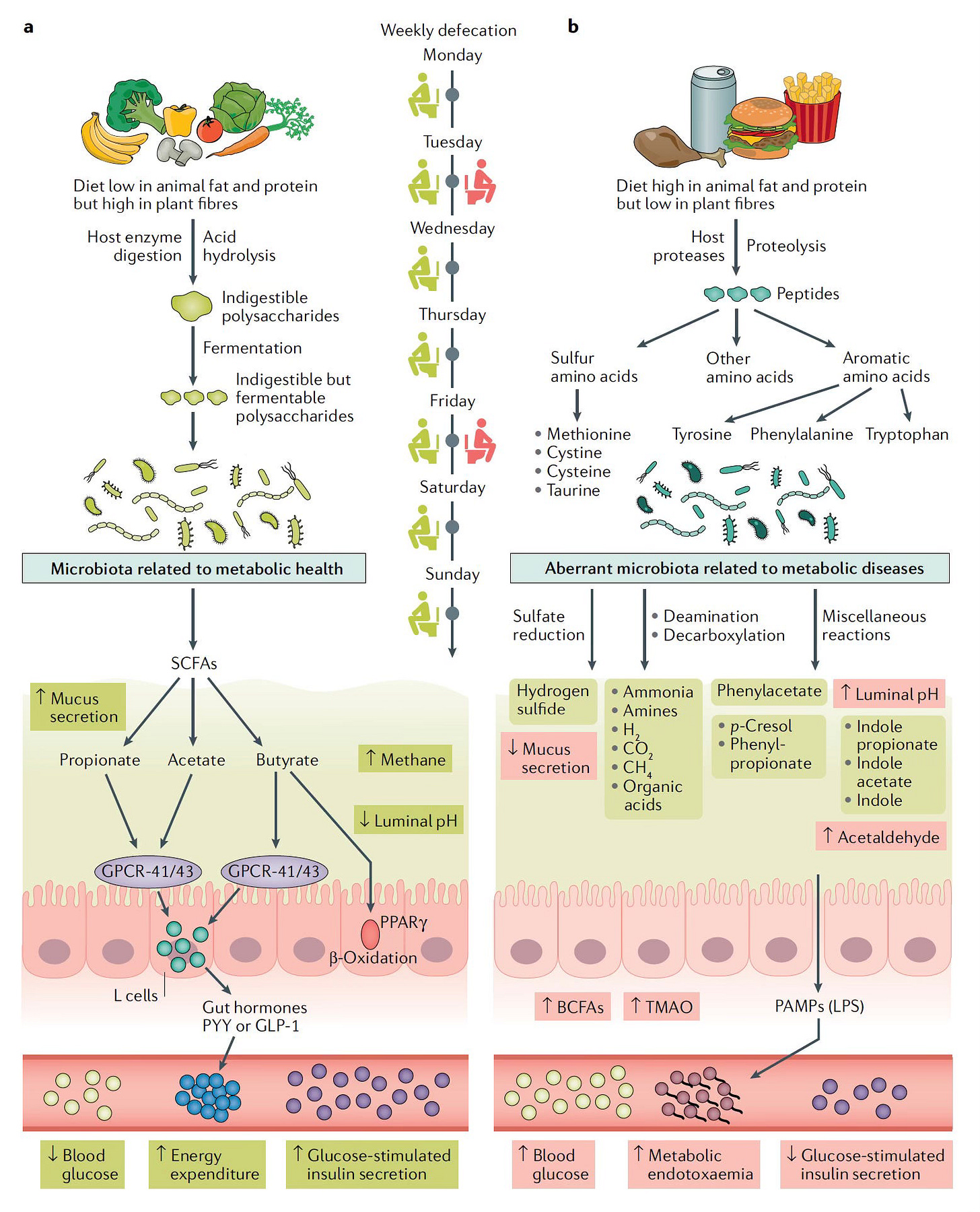
Our diet plays a major role in the gut microbiome's composition and how it works on our behalf. Our beneficial intestinal passengers and collaborators thrive upon high-fiber, plant-based foods, such as whole grains, seeds, tree nuts, legumes (beans, pulses, peanuts), root crops (carrots, beets), and cruciferous vegetables (broccoli, Brussels sprouts). While it’s not yet possible to “rewild” your gut’s microbiome, you can certainly improve it.
Dietary fiber is an outstanding prebiotic. You don’t need to take prebiotic supplements if you eat a healthy diet, with the possible exception of psyllium fiber. While no official definition exists for high-fiber foods, some experts suggest applying it to foods containing at least 5 grams of dietary fiber per serving. Because such foods can also be high in total carbohydrates, it is important to consider a food’s fiber density.
It is the absence of insoluble fiber, coupled with a high free-sugar content, that makes the touted three-day “juice cleanse” regimen harmful for the gastrointestinal microbiome. According to a 2025 study, the relative abundance of bacteria associated with inflammation and gut permeability increased as a result. It may take a couple of weeks for the microbiome to recover from the insult. So much for another so-called “wellness” fad.
Prioritize high-fiber foods that have at least one gram of dietary fiber for every five grams of total carbohydrates (and no more than one gram of total sugars per 10 grams of carbs), or several grams of fiber for every 100 calories. For most packaged, multi-ingredient foods such as whole-grain cereals, pasta, and breads, aim for a fiber content that is close to, and preferably higher, than the total sugar content.
For example, my favorite cracker, Wasa Multigrain Crispbread has 45 calories in each 14 gram cracker, with 11 grams total carbohydrates, 3 grams of dietary fiber (including 1 gram of soluble fiber), and zero total sugars. As a bonus, it has 2 grams of protein per cracker. If you can find a healthier cracker, please let me know about it.
The effects of beta-glucan consumption, a soluble fiber found in grains such as oats and barley, resemble some of the benefits seen with GLP-1 receptor agonists (GLP-1 RAs) like Ozempic. These drugs work by mimicking a hormone called glucagon-like peptide-1 (GLP-1), which helps to regulate appetite and blood sugar levels. Dietary beta-glucans stimulate the release of naturally occurring GLP-1s in the gut, ie. the moniker, “Nature’s Ozempic.”
Focus on a Diversity of Plants
While you’re increasing your fiber intake, it is also important to diversify the sources of that fiber. A broad variety of fruits and vegetables provides other nutrients that are essential for a healthy gut microbiome. Hence the saying, “Eat a rainbow of produce.” There is an “entourage effect” that occurs when different micronutrients work together in complementary ways.
Our gut microbiome appears to welcome the company of probiotic bacteria found in fermented foods such as yogurt, kefir, sauerkraut, and kimchi, although it is not clear how many actually survive to reach the small and large intestines. On the other hand, we will want to avoid foods that can adversely impact our intestinal flora. That includes foods with added sugars, and particularly foods high in fructose, such as table sugar, honey, and maple and agave syrups.
If you want to be kind to your microbiome (and of course you do), you are encouraged to avoid artificial and so-called “natural” low-calorie sweeteners. Erythritol and other sugar-alcohols, once considered benign sugar substitutes, can disrupt the gut microbiome. Because humans and their microbiomes co-evolved as a symbiotic partnership, ingestible substances that were not part of the early hominid diet are likely to not be well tolerated by the organisms that comprise a health-promoting gut microbiome.
Stevia leaf extract has received both positive and negative conclusions from studies looking at gut microbiome disruption. The most recent review (2022) of in-vitro and in-vivo studies concluded that “Alterations in the colonic microenvironment may depend on the amount and frequency of stevia intake, as well as on the simultaneous consumption of other dietary components.” Keep in mind that there is a great deal of variability among Stevia products, some of which may or may not have an impact.
To be on the safe side, I suggest minimizing the consumption of refined carbohydrates such as white flour and white rice, highly saturated and trans fats, processed meats, and avoiding all ultra-processed food products (UPFs) containing non-nutrient food additives, and especially those containing preservatives, emulsifiers, bulking agents, and food dyes.
Emulsifiers have been shown to break down the protective mucus barrier between the gut bacteria and the cells that line the colon. Carrageenan, extracted from seaweed and concentrated, is a common emulsifier found in UPFs. Your microbiome also hates alcohol, NSAIDs, and too much salt. A recent analysis of fecal microbiome signatures showed significant differences among different kinds of diets and their associated health outcomes.
Plan your meals around a plant-based, diverse, omnivorous diet. Start with foods that are high in fiber, such as whole grains, legumes (beans and pulses), seeds, and nuts. Next, includes a wide variety of fresh fruits and vegetables. Then, make sure your meals contain an adequate amount of high-quality protein, and you’re good to go!
In addition to our own nutrition, we need to consider the care and feeding of our gut microbiome and keeping our symbiotic intestinal passengers happy so they will continue working to our benefit. Don’t mistreat them with salt, sugar, and the chemicals found in ultraprocessed foods. Resistant starches also contribute to microbiome health in ways that are similar to those of fiber.
Out the Other End
Everybody poops, but for most people, it’s not every day. Younger people, women, and those who are skinny, tend to have less frequent bowel movements. Research suggests that bowel movement frequency is linked to long-term health. If stool stays too long in the gut, the resident microbes use up all of the available dietary fiber, and stops converting it into beneficial short-chain fatty acids. After the fiber is gone, the gut ecosystem switches to fermentation of proteins, which produces several toxins that can make their way into the bloodstream.
A bowel movement once or twice a day is considered optimal. A fiber-rich diet, good hydration, stress reduction, adequate sleep, and regular exercise all contribute to pooping on a regular basis. In a generally healthy population, constipation is associated with blood levels of microbially derived toxins prior to any disease diagnosis. If you’re constipated, lifestyle interventions are far preferable to taking laxatives. However, if from time-to-time you need a little supplemental assistance, magnesium citrate USP and psyllium fiber are both recommended.
The bacteria associated with protein fermentation tend to be more populous in people with constipation or diarrhea. Protein fermentation by-products known to cause damage to the kidneys, such as p-cresol-sulfate and indoxyl-sulfate, were found in the blood of individuals reporting constipation, while clinical chemistries associated with liver damage were elevated in individuals reporting chronic diarrhea.
Forget Probiotic Supplements
Bacteria-containing probiotic supplements are unnecessary. A recent study showed no consistent benefits for probiotics in treating metabolic syndrome. In rare instances, probiotics might be prescribed for specific medical conditions, but don’t waste your money on unregulated, over-the-counter probiotics. While generally considered safe, harms have been reported.
Claims made by the probiotic supplement industry are not supported by any reputable research. A few randomized controlled trials (RCTs) of probiotics have been conducted or sponsored by the manufacturers of those products, and their self-serving results cannot be trusted due to conflicts of interest.
Postbiotics are non-microbial substances produced as waste products by beneficial bacteria in the gut. Some of them, such as short-chain fatty acids and vitamin K, have beneficial health effects. As might be expected, they are also being hyped by the supplement industry. You are better off obtaining postbiotics from fermented foods such as sauerkraut, kimchi, and kefir.
Capitalizing upon people’s gullibility, companies have developed products alleged to enhance the gut microbiome. Since these products are not considered drugs, the FDA cannot regulate them or limit most such claims. Convincing evidence for any supplements helping with specific conditions is mostly lacking, with the exception of those used to treat vitamin or mineral deficiencies.
The ecology of the gut microbiome is exceedingly complex, and the relationship between probiotics in supplements (and fermented foods), and whatever impact they might have upon the gut’s microbial population, is poorly understood. Nonetheless, many companies are eager to cash in on exaggerated claims about the value of fecal microbiome sequencing and an already huge demand for probiotic products.
Research suggests that taking probiotic supplements, whether intended to boost health or to counter the effects of taking antibiotics, can crowd out some of the beneficial gut microbes and reduce microbiome diversity. Intestinal dysbiosis (an imbalance of the gut microbiome) has been linked to a number of health problems. Bottom line: Don’t take probiotic supplements.
Fermented Foods
There are many good reasons to eat fermented foods. They taste good, and are part of our biological heritage. The transition of early hunter-gatherers to agricultural communities required food preservation. Archaeological evidence shows that humans have been preserving vegetables by fermenting them for at least 6,300 years. Genomic analysis suggests that our association with fermented foods dates back to a time when the evolution of our hominid ancestors diverged from that of the other primates, a very long time ago.
Homemade lacto-fermented pickles and sauerkraut are a lot healthier than what is typically found in grocery stores. However, there isn't convincing evidence for any specific health benefits from the consumption of fermented foods. Eating them to modify your gut microbiome, or to treat or prevent any specific health conditions, should not be one’s goal.
Despite a recent deluge of claims by online influencers and people with something to sell, convincing evidence for any specific health benefits attributable to fermented foods is woefully lacking. However, research in this area is still very much in its infancy.
Fermented foods could potentially modulate both the composition and the functionality of the human gut microbiome, according to a 2024 review. However, the direct transfer of microorganisms from fermented foods to the human gut remains unproven. The health benefits of fermented foods may be more related to the novel compounds produced by the fermentation process, such as short-chain fatty acids and bioactive peptides.
Some of the microbes in fermented foods are able to survive gastric transit and could presumably affect the gut microbiome by inhibiting or competing with the existing species. Transient or long-term colonization of the gut by live microbes in fermented foods, and the impacts upon the indigenous gut species, are areas in need of further study.
Some lactic acid producing species of bacteria found in fermented foods, such as Lactiplantibacillus plantarum, can directly contribute to the intestinal population, while others seem to have little or no impact. Those that are able to survive the transit through the human digestive system might or might not become established in the large intestine, either temporarily, or for the long term. The impact on the microbiome of the small intestine is much more difficult to study.
At the present state of our knowledge, fermented foods seem less likely to modify the gut microbiome through their direct bacterial contribution than they do by providing certain nutrients, such as polyphenols, that enhance the growth of certain species within the pre-existing microbial population. If one’s intention is to directly alter the composition of the gut microbiome, the most effective way is via fecal microbial transplants.
According to a recent study, transplants targeting the small intestine were more effective than those impacting the large intestine, when it comes to the treatment of irritable bowel syndrome (IBS). Researchers will need to learn a lot more about many aspects of the gut microbiome before doctors can feel confident about significantly altering it through various interventions.
It does seems possible that fermented foods could exert a greater influence upon the microbiome residing in the small intestine, rather than the large intestine. However, because it is much more difficult to investigate microbial populations in the small intestine than it is to analyze stool samples, there is a paucity of data in that regard. The hypothesis that the impact of fermented foods on human health is due to its ability to alter the small intestine microbiome certainly deserves further investigation.
A recent study involving the regular consumption of lacto-fermented vegetables (LFVs) has shown that they have only a slight effect on the bacterial composition of stool samples. LFVs had a much greater effect on the amount of short-chain fatty acids (SCFA), especially butyrate, produced by the microbial fermentation of dietary fiber in the large intestine. This occurred mainly as a result of the vegetables themselves serving as nutritional “prebiotics” for the intestinal microbiome, although lacto-fermentation does produce SCFAs.
Butyrate and other SCFAs have been shown to have important biological activity, including a supply of energy to the cells lining the intestine, thereby protecting the mucosal barrier. SCFAs play a role in modulating immune responses toward an anti-inflammatory state, and reducing oxidative stress. Butyrate also plays a direct role in preventing fatty liver disease. The advantage of using fiber-rich prebiotics to enhance intestinal butyrate production is that it occurs at the right time, and in the right place, to do the most good.
Supporting our natural intestinal sources of butyrate through our diet seems like a good way to go, regardless of whether the foods are lacto-fermented or not. At the same time, it would also be prudent to avoid ingesting substances known to produce dysbiosis, such as junk foods high in sugar, salt, and fat, ultra-processed “fake foods,” sweeteners, alcohol in any amount, NSAIDs such as aspirin, ibuprofen, and naproxen, and taking unnecessary antibiotics for virus infections.
In a Pickle
Cucumbers are thought to have originated in India in the Himalayan foothills. Archeologists and anthropologists believe that the ancient Mesopotamians employed pickling practices around 2400 BCE, from a necessity to preserve food. Pickling likely developed independently in multiple regions around the world. There is evidence that people living in the Tigris Valley, now in present-day Iraq, were pickling cucumbers brought from India around 2030 BCE.
National Pickle Day is celebrated on November 14, but you can enjoy the prickly-sour taste of pickled cucumbers, gherkins, and cornichons any day of the year. Commercially made pickled fruits and vegetables are produced either by fermentation in a salt-water solution or by soaking them in a vinegar solution. Only fermented, unpasteurized pickles contain probiotic bacteria.
The jars of vinegar-pickled cukes found on grocery store shelves usually contain preservatives such as polysorbate 80 and sodium benzoate, both of which should be avoided if you want to maintain an amiable relationship with your gut microbiome. However, vinegar pickling is really easy to do at home, and does not come with the downside of adding copious amounts of sodium to your diet, the way that brine pickling does. Simply make a 1:1 vinegar to water solution, using vinegar with at least five percent acetic acid content.
The upside of pickling with brine is that “lacto-fermentation” involves the proliferation of potentially beneficial bacteria, while vinegar pickling kills bacteria and prevents fermentation from taking place. Unfortunately, there are very few brands of commercially produced fermented pickles (kept in the store’s refrigerated case) that will actually contain live, active cultures of probiotic bacteria, so check the ingredients labels carefully.
Fermented pickle aficionados may need to do a lot of sweating to get rid of the excess salt, but vigorous exercise and saunas can be good for you. Check with your doctor first. When it comes to salty foods such as pickles and sauerkraut, I advise moderation.
There are lots of other vegetables that can be lacto-fermented, such as beets, cabbage, carrots, cauliflower, garlic, green beans, kohlrabi, peppers, radishes, snap beans, tomatoes, turnips, and zucchini. If you're interested in doing your own pickling, the book I recommend is “Fermented Vegetables.” It’s author has a presence on Substack.
I suggest that you start you fermentation adventure with pickled cucumbers. They are actually quite easy to produce, and make a great snack. I like to eat them in sandwiches made with whole-grain bread, natural peanut butter, and cheese. If you are a subscriber, and would like a free copy of my pamphlet on pickle-making, reply to any of my emailed newsletters and request it.
This Post may be updated at any time. Please check back here again to find the latest information on this subject.
Find more articles about Healthy Living in my Post Archive.
Please share my Website Link with others via your social media accounts.
You can help your friends and followers become healthier by suggesting that they subscribe to this Newsletter. You may receive access to premium features as a thank-you for making referrals:
If you find this Newsletter to be of value and want to lend your support, please consider making a donation that will help it reach many more people: