UPDATED: February 12, 2025
Welcome to the Healthy Living Is Good Medicine Newsletter, a totally free, health education publication covering a wide variety of topics with original articles intended to help people lead healthier and more fulfilling lives.
Why write about a disease that is rare in the United States? Well, for one thing, Americans travel to other parts of the world, where they can be exposed to endemic tropical diseases:
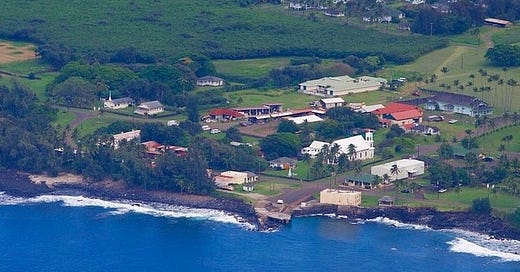
Leprosy (aka “Hansen’s Disease”) is an infectious disease caused by a relative of the tuberculosis bacteria and is transmitted via droplets from an infected person's nose and mouth. The other reason for my interest is that I was the last resident physician to take care of the leprosy patients in Kalaupapa, Hawaii, on the island of Molokai:
My Experience with Leprosy
While it's unusual for an American to bring home leprosy as a travel souvenir, a friend of mine went on a yoga retreat in India and became infected while there. Sadly, his immune system was unable to fight off the infection, and the disease progressed very rapidly. He also had great difficulty tolerating the necessary treatment.
After that initial encounter with someone who actually had leprosy, I acquired an in-depth experience with the disease when I later took a position with the Infectious Disease Division of the Hawaii Department of Health. I was appointed Medical Administrator of the Kalaupapa Leprosy Settlement on the Island of Molokai.
As the only full-time physician in residence, I supervised the clinic and small hospital, while caring for Kalaupapa's leprosy patients. At one time, they all had been forcibly quarantined there in an effort to prevent the spread of the disease. My time in Kalaupapa was a truly extraordinary experience. It came to an end when State budget cuts and a declining patient population made my position no longer cost-effective.
Public health efforts in Hawaii date back to 1850, when the Privy Council of King Kamehameha III established the Board of Health for the Kingdom of Hawaii. In 1854, the Hawaiian government made smallpox vaccination compulsory. In 1865, King Kamehameha V set aside the land that is now Kalawao County on the Island of Molokai for the mandatory confinement of leprosy patients, a policy remained in effect for the next 103 years.
Many people complained loudly about the mask and vaccine mandates that were instituted during the height of the COVID-19 pandemic. Compare that to being removed from one’s family and forced into quarantine on a remote island peninsula. For more than a century, that’s exactly what happened to Hawaii’s leprosy patients.
On August 21, 1959, Hawaii became the 50th American state. The following year, the “State of Hawaii Reorganization Act” established the Department of Health. In 1969, following the development of effective antibiotic treatments that rendered the disease non-contagious, the state’s mandatory quarantine policy was rescinded.
Because the patients no longer posed a public health threat, they were free to come and go as they pleased. However, most of them still suffered lingering disabilities due to the damaging effects of their illness. When I arrived in Kalaupapa in 1993, they were suffering the typical infirmities that accompany advancing age. Very few of them are alive today.
Etiology
Infection with either Mycobacterium leprae or Mycobacterium lepromatosis can produce the disease, resulting in damage to the peripheral nerves, skin, muscles, upper respiratory tract, and eyes. Both are related to the organism that causes tuberculosis. Mycobacterium leprae was discovered in 1873 by the Norwegian physician, Gerhard Armauer Hansen. It was the first bacterium ever to be identified as the cause of a human disease. The organism is an obligate intracellular pathogen, and cannot be grown in typical laboratory culture media.
Transmission
Leprosy is transmitted through repeated close encounters with an infected person, and is typically spread when their bacteria-laden secretions come into contact with another person's mucous membranes. This occurs primarily through respiratory droplets, such as those produced by coughing or sneezing. The organism has a very low infectivity rate, and only five percent of people who are exposed to M. leprae develop the disease.
People in the continental United States have become infected after contact with nine-banded armadillos that inhabit the Gulf coasts of Texas, Louisiana, and Florida. It is hypothesized that the armadillos, which are an especially susceptible species, first acquired the leprosy from early European explorers of the Americas.
Leprosy eventually became well established in the armadillo population. Today, up to 20 percent of the southeastern armadillos carry the the bacteria. Because it can be transmitted from animals to humans, leprosy is considered a zoonotic disease. In the wilds of Africa and India, leprosy has been found in primates such as chimpanzees and macaques.
A National Leprosarium was established in Carville, Louisiana, in 1917, and operated until 1999. Outpatient clinics were created in 1981. The National Hansen's Disease Program currently provides care, facility coordination, research, and information about the disease. There were 225 new cases of leprosy reported in the U.S. in 2023.
Diagnosis
Early diagnosis and treatment are crucial in preventing disability and transmission, although it can take as many as 20 years for symptoms to appear in some people. The incubation period usually ranges from a few months to several years, which can make diagnosis challenging. Most commonly, an anesthetic patch of skin will be the first sign of an infection, and usually appears within a year. A laboratory-confirmed diagnosis requires a skin or nerve biopsy.
Leprosy's typical skin lesions can appear as pale, reddish, or brownish patches that eventually lose sensation. Palpable swelling or thickening of the ulnar and greater occipital nerves can occur. Noticeable lumps or nodules on the face, ears, trunk, and extremities are typically seen in the advanced stages of lepromatous leprosy, characterized by widespread skin involvement and large numbers of bacteria in the lesions. It can eventually result in thickened skin on the forehead, nose, ears, and chin, producing what is known as leonine facies.
Peripheral nerve damage often affects a person's ability to feel pain, and can cause muscle weakness and paralysis. Numbness in the hands and feet can result in injuries going unnoticed, leading to wound infections and sometimes necessitating amputations. Severe cases cases of leprosy can damage the eyes and cause blindness.
Genetic factors, the number of infecting organisms, and the immune system's response to infection all play a role in both the susceptibility to and progression of the disease. Once infected, the presentation and severity of leprosy's symptoms varies, depending upon the individual's immune response.
Three forms of the disease are recognized: Tuberculoid leprosy is characterized by a strong immune response, resulting in a limited number of skin lesions and less nerve damage. Lepromatous leprosy is associated with a weak immune response, leading to widespread skin lesions, nerve damage, and potential organ involvement. Borderline leprosy, also known as dimorphus leprosy, is due to an intermediate immune response, and displays the features of both the other types.
Treatment
While once greatly feared and misunderstood, leprosy is now a treatable and curable condition. Treatment involves a multi-drug regimen, with a combination of dapsone, rifampicin, and clofazimine, in order to combat antibiotic resistant strains and prevent the emergence of new resistant mutations. The three drugs are administered in accordance with the recommendations of the World Health Organization (WHO). This combination of antibiotics first inactivates, and then kills the Mycobacterium bacteria.
Early and consistent treatment will cure leprosy and prevent further complications. However, nerve damage that has already occurred may not be reversible. Even the most severe cases of leprosy become non-infectious within a few weeks of treatment. In the U.S., the treatment specified by the CDC can take one to two years in order to effect a complete cure, depending upon the severity of the disease, which is classified as either paucibacillary or multibacillary.
Leprosy's History
Despite significant advances in medical science, leprosy continues to affect millions of people worldwide, primarily in developing countries. Its long, complicated, and often sordid history dates back thousands of years. Ancient civilizations, including those in Egypt, India, and China, described the widely feared disease, which was often associated with spiritual impurity and divine punishment. A religious and social stigma has persisted throughout history, leading to forced isolation and severe discrimination against people with the illness. The term “leper” is considered pejorative.
In the Middle Ages, leprosy reached epidemic proportions in Europe, prompting the establishment of leper colonies to isolate infected individuals. These colonies, known as leprosaria or lazarettos, were often located outside city walls. They became symbols of fear and discriminatory persecution. While the disease declined in Europe over time, it continues to be a significant health problem in other parts of the world, such as Southeast Asia, India, Africa, and South America.
How this mutilating and debilitating disease came to Hawaii is unknown, but at the time it was blamed on Chinese immigrant laborers. It was first recorded in Hawaii during the 1830s. Native Hawaiians, lacking immunity to introduced diseases, were particularly susceptible to infection and vulnerable to its worst consequences. Fearing its spread, King Kamehameha V signed into law the “Act to Prevent the Spread of Leprosy” on January 3, 1865.
Police were required to track down and arrest people suspected of having the disease. They were then taken to Kalihi Hospital and Detention Station in Honolulu for evaluation. Patients in the early stages of the disease were given experimental treatments. Those with more advanced disease were sent to Kalawao on the windward side of a five square mile peninsula on Molokai Island’s north shore. In 1889, the patients were moved to Kalaupapa on the leeward side, because of its more hospitable climate.
Surrounded by rough seas and walled in by some of the highest sea cliffs in the world, patients imprisoned on the peninsula had little chance for escape. Some patients did manage to scale the 3,000 foot cliffs before being apprehended. Natives living on the peninsula were relocated before the arrival of the first leprosy patients. Due to its topography, the fierce resistance of its inhabitants, and the legendary black magic of its sorcerers, Molokai was never conquered by Hawaii's warrior kings, and was mostly avoided by rest of the Hawaiian population.
During the period of mandatory confinement, more than 8,000 patients were sent to Kalaupapa Settlement. On December 22, 1980, President Jimmy Carter established part of the peninsula as the Kalaupapa National Historical Park, and restoration of many of the settlement's structures began. The house in which I lived while there had been the doctor's residence for over a century.
Contrary to the tall tales fabricated by the patients in order to garner sympathy and donations, they were never thrown overboard and forced to swim ashore through shark-infested waters. When the first patients arrived in 1866, the infrastructure was already in place, and they never had to struggle to survive. FYI, the Hawaiians have a saying: “Never let the truth get in the way of a good story.” Apparently, James Michener fell for those fabrications, and included them in his novel, Hawaii.
In 2009, the canonization of Father Damian brought worldwide attention to Kalaupapa. In 1873, the priest set about making Catholic converts in the settlement, while helping with community improvements and tending to the people’s individual needs. As a result of his close contacts with the patients, he was diagnosed with the disease in 1884, and died in 1889.
Leprosy Today
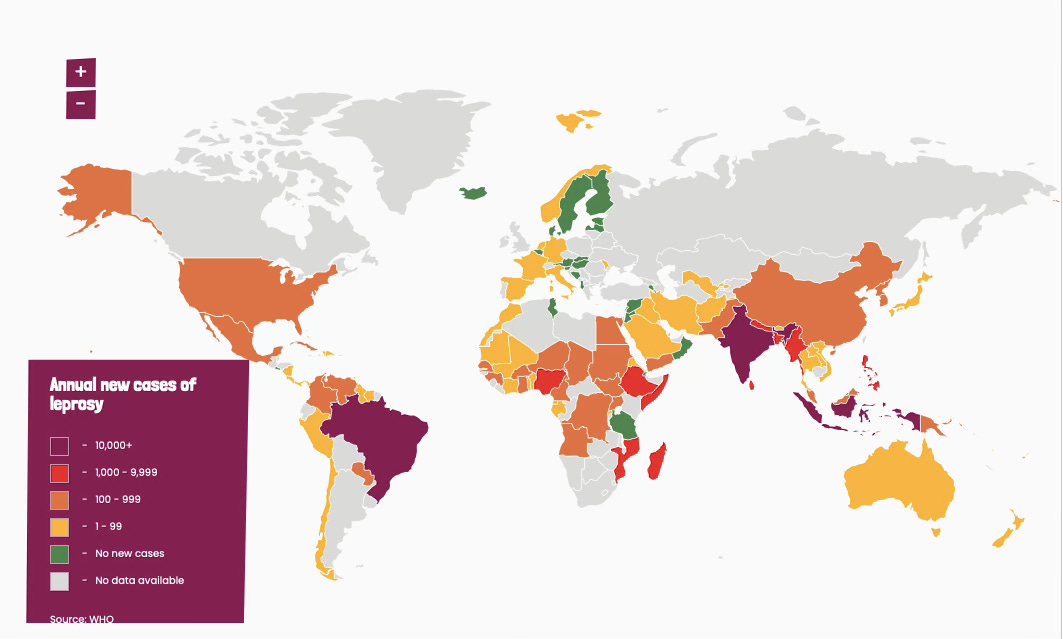
Currently, there is an estimated 1.15 million leprosy cases worldwide, distributed over more than 120 countries. About 200,000 new cases are reported every year. The WHO has made significant progress in combating leprosy through its global efforts to provide free, multi-drug treatment to affected individuals, and by raising general awareness about the disease. As a result, the number of new leprosy cases has decreased dramatically in recent decades. We shall have to see what happens, now that Trump has withdrawn U.S. financial support for the WHO.
Many challenges remain, particularly in regions with limited access to healthcare, and those with persistent stigmatization of the afflicted. This stigma can exacerbate the psychological and social impacts of the disease, hindering patient recovery and reintegration into society. There are ongoing strategies to end discrimination against people living with leprosy through public education, community acceptance programs, and from the patients' own demands for their basic human rights.
Continued efforts are needed to eliminate leprosy as a public health problem, and to ensure that people with the disease receive all the care and support that they need. The Kingdom of Jordan has recently been recognized as the first country in the world to completely eradicate leprosy.
― ― ―
These Posts can be updated at any time. Please check back here again to find the most up-to-date information.
Find a lot more of my articles about Healthy Living in my Post Archive.
Be sure to share my Website Link with others via your social media accounts. You can help your friends and followers become healthier by suggesting that they subscribe to my totally free Newsletter.