UPDATED: June 3, 2025
Welcome to the Healthy Living Is Good Medicine Newsletter, a totally free, health education publication covering a wide variety of topics, with original articles intended to help people lead healthier and more fulfilling lives.
Presaged by my previous article about pain and suffering, I’t is with a heavy heart that I’ve been helping a loved one with Alzheimer's disease (AD) transition to the memory care unit of an assisted living facility. If you've ever been in a long-term relationship with someone who develops dementia, you know how devastating this disease can be as it progressively diminishes their intelligence and destroys their personality.
During my career as a physician, I have witnessed many gruesome illnesses and injuries. I can now say that dementia is among the worst of them. Watching someone progressively deteriorate as amyloid plaques and neurofibrillary tangles in their brain relentlessly destroy their cognitive abilities is especially difficult when it happens to someone with whom we are close. Given the choice, I’d rather look away.
Disease Progression
The personality changes that people with dementia initially undergo remind me of a 1978 sci-fi horror film, “Invasion of the Body Snatchers.” After an earthling's body has been hijacked by aliens, they outwardly appear the same, but who they are becomes disturbingly different.
For those with AD, short-term memory is usually the first thing to go. They will ask the same question over and over again, because they can’t remember your answer. As their self-care abilities and sense of humor evaporate, they start saying and doing things that make no sense.
Delusions and hallucinations are experienced by at least a quarter of those with Alzheimer’s disease, and the appearance of psychotic features heralds an acceleration of cognitive and functional decline. As the disease progresses, communication becomes increasingly difficult.
Eventually, they will no longer recognize you, and don’t know who they are. Alzheimer’s is a terminal illness, but the bigger tragedy is that the person we know and love will be gone long before their disease becomes fatal. Its clinical course eventually impacts a person’s physical functions, and late-stage caregiving can be very challenging and require hospice support.
We need to allow our loved ones to expire peacefully, especially when those with dementia are among the living dead. “Do Not Resuscitate” (DNR) orders and an Advance Medical Directive are a necessity, if we don't want them tortured by medical and surgical interventions at the end of their life.
Losing Our Selfhood
As if the infirmities and indignities of old age aren’t bad enough, dementia strikes at one of our deepest fears: loss of control over our own minds. We typically define ourselves by our memories and thoughts, and dementia does not simply impair them; it dismantles our sense of self from within.
Becoming aware that our mind is slipping away can produce moments of intense terror and profound sadness. There are flashes of self-awareness when we realize that something is wrong, and know that we are losing our grip on reality. At those times, the threat can feel existential. As the disease progresses, we mercifully become less aware of our plight.
The unique cruelty of Alzheimer’s disease, compared to other terminal illnesses, lies not only in its progressive deterioration of memory, but also in how it erodes the very foundations of a person's identity and emotional connection with others, long before their body fails. It destroys their intelligence, corrupts their autonomy, ruins their relationships, and hollows out their personality. The disease ruthlessly dismantles a person's identity and connections in a way that no other illness exacts with such devastating precision.
Regardless of its etiology, dementia is essentially a thief that insidiously and invisibly robs us of who we are. At first there is forgetfulness; we don't remember where we put something, start missing appointments that aren't written down, or are unable to recall the names of acquaintances and once familiar objects. Eventually, the disease steals our life stories and our ability to recognize the people we love. Even our own face in the mirror becomes unfamiliar.
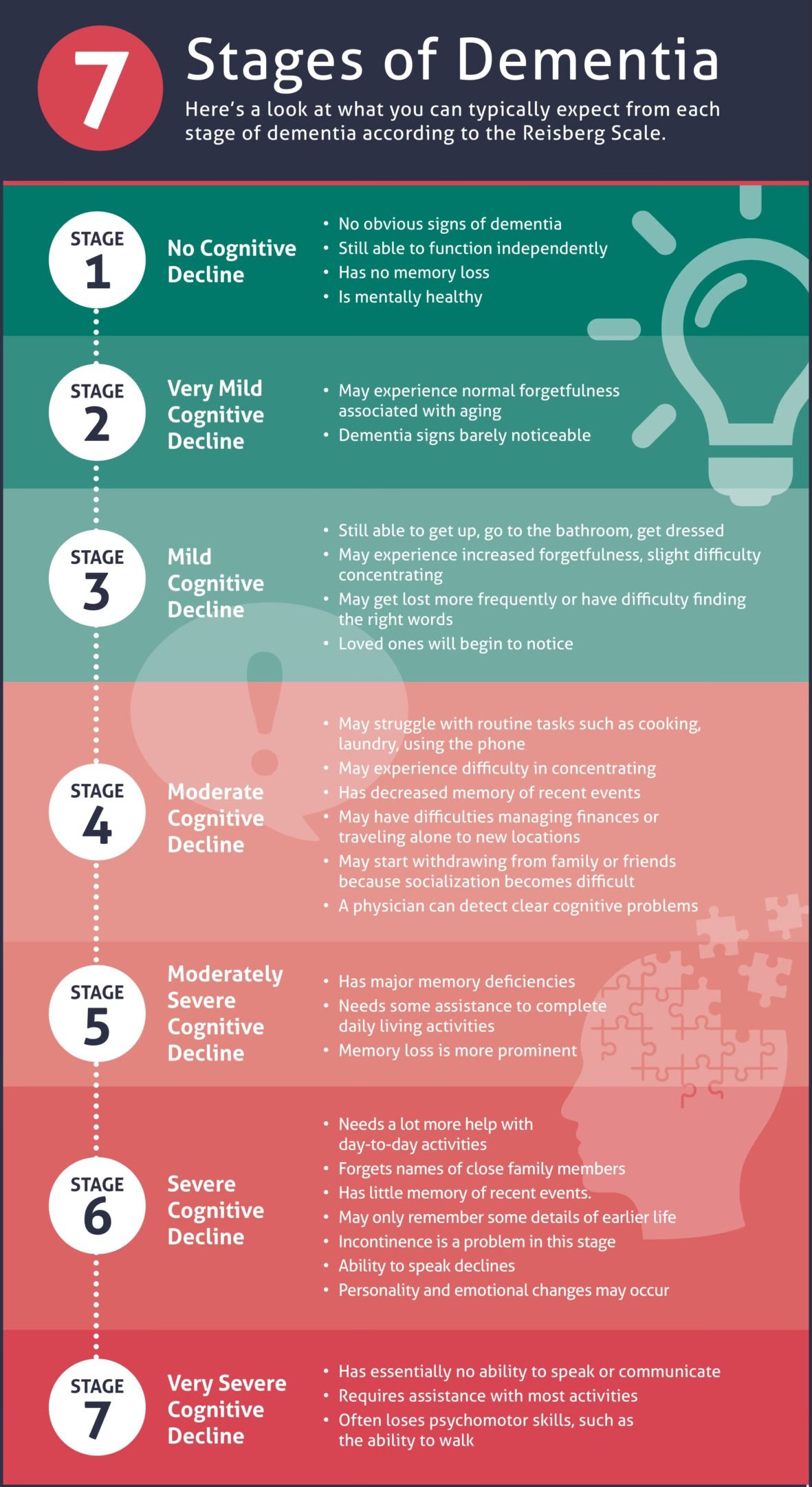
To that I would add Stage 8: Terminal. Death typically occurs due to complications, rather than the disease itself directly causing it. The most common causes of death is infection, particularly pneumonia. This happens when the person loses their ability to swallow properly (dysphagia), leading to aspiration of foods, liquids, or saliva. Their immune system is also weakened, making it harder to fight off infections. Unrecognized urinary tract infections can quickly become life-threatening.
As people lose their ability to move independently, this can lead to blood clots and decubitus ulcers (bedsores) with their associated risk of systemic infections. As eating and swallowing become increasingly difficult, many people lose significant weight, develop malnutrition, and may become dangerously dehydrated, despite careful care.
The dying process in late-stage Alzheimer's is typically a gradual decline rather than a precipitous event. Many people become increasingly frail, sleep more, eat and drink less, and continue to withdraw over a period of weeks or months. Comfort measures provided by palliative and hospice care can keep people comfortable and enable them to pass more peacefully. Additional details about the terminal phase of AD can be found here.
The Toll Upon Caregivers
Long before the terminal phase, watching someone who you know and love slowly unravel and eventually disappear is part of what makes Alzheimer’s especially painful for others. Of all the illnesses that involve caregiving at home, AD takes the greatest toll upon the caregivers, and produces its own unique kind of grief.
The loved one is both present and absent at the same time. Their body may still be strong, their smile still appears warm, but behind their eyes a once familiar personality is no longer present. For families and caregivers, that creates a haunting ambiguity. They will have to grieve the loss of someone who is not yet gone, love someone who cannot love them back, and try to hang on to the brief periods of lucidity that flicker in and out, tempting them to pin their hope on small improvements that never last.
Unlike diseases that affect the body alone, Alzheimer’s attacks the heart of people's relationships, their human dignity, and their ability to meaningfully engage with the world. It burdens families with overwhelming decisions and imposes a buden of long-term caregiving that is physically exhausting, financially draining, and emotionally heartbreaking. In its later stages, when the ability to communicate is gone and emotional connections are shattered, unpaid caregivers can bear the additional weight of guilt for wishing that the unbearable load they are carrying will soon come to an end.
Something that may help with the emotional burden that comes with taking care of a loved one with dementia is the belief that at a deeper level there is still a silent connection. What follows is adapted from a mother’s letter to her son, found in The Caregivers Helpbook (page 37).
“If there comes a time when I am unable to recognize you because of my disease, know that my essence will always be present. Even though I may not be, in body and mind, the person you once knew, I am still with you. We may not be able to talk with each other as we once did, but if you play music and we sing together, or we take a walk holding hands, or if you just sit quietly next to me, I will feel your love, and you will feel mine.”
The Dementia Epidemic
A major cause of disability among older adults, Alzheimer’s disease was the seventh leading cause of death in 2022, according to the CDC. Alzheimer’s Association estimates are that 6.7 million Americans age 65 and older have the disease. That’s 10.9 percent of the senior demographic. About two-thirds of Americans with Alzheimer's are women. The prevalence of AD sharply increases with advancing age.
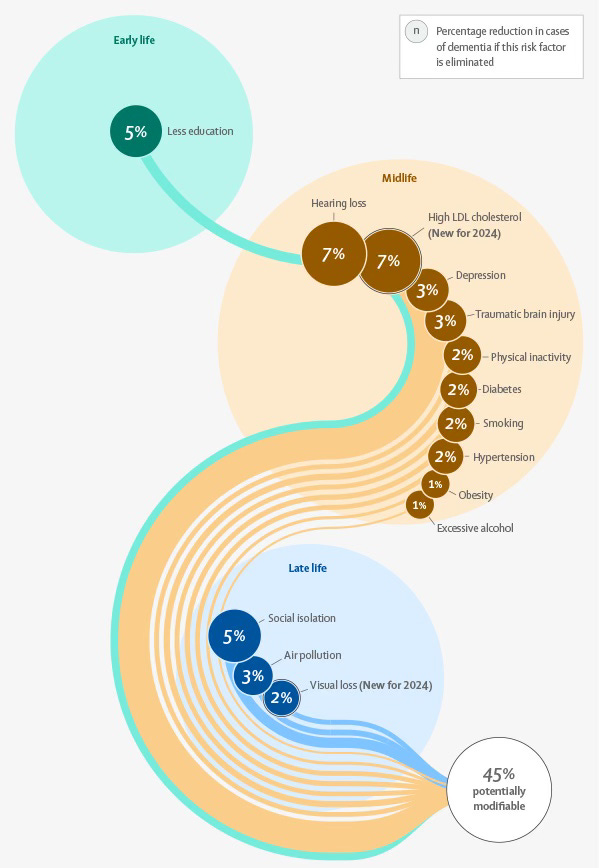
Alzheimer’s disease accounts for about 65 percent of all dementia cases, and is considered a global public health emergency. It has been suggested that up to 45 percent of AD cases could be prevented, mitigated, or delayed by addressing modifiable risk factors, in part through healthier lifestyles. In this article, I will focus upon lifestyle interventions that may slow the progression of Alzheimer's disease, such as diet and exercise. Maintaining a healthy weight, engaging in regular physical activity, and medically treating contributors to the metabolic syndrome are crucial.
Aside from a genetic predisposition, the most prominent modifiable risk factors for Alzheimer disease and related dementias are mid-life obesity and physical inactivity. Smoking, depression, diabetes, midlife hypertension, hearing loss, and being poorly educated are also major contributors. A history of concussions, excessive alcohol consumption, and long-term exposure to fine particulate air pollution are also known to increase AD risk.
Neurodegenerative diseases including AD are about equally attributable to genetic risk factors present at birth and environmental influences that can potentially be avoided or ameliorated. A recent study has uncovered a link between ultra-processed foods (UPFs) and dementia. Researchers found that a 10 percent increase in UPFs was associated with a 16 percent higher likelihood of developing cognitive impairment. This increase was seen even in individuals who otherwise adhered to healthy diets.
There's a lot more that can be said about dementia's diagnosis, prognosis, medical treatment, and psycho-social interventions. The brain’s glymphatic system and its role in neurodegenerative diseases is an exciting new area of research. A new blood test for the p-Tau217 biomarker is a major diagnostic and prognostic breakthrough. It is able to determine with almost total accuracy if Alzheimer’s disease pathology is present in patients’ brains, and can predict when their symptoms of mild cognitive impairment will appear. It can also be used to monitor the effectiveness of treatments intended to reduce amyloid plaques.
Interestingly, according to a recent systematic review of eight randomized, controlled trials, music therapy can improve cognitive functions in patients with Alzheimer’s disease. What I have observed with my loved one is that when I sing and play guitar, she can remember the lyrics and sing along. For a period of time afterward, she is more present and engaged.
Much more research will be necessary to assess the neurobiological effects of music therapy, determine the best intervention strategies, and optimize the therapy’s long-term effects. For now, the institutional challenge involves finding an escort so my loved one can attend the twice-weekly live music performances, and to help her select music that she can listen to when she is alone in her room.
Quack Treatments
It's crucial to understand that there is currently no cure for Alzheimer's disease. The treatments available aim to manage symptoms, and in some cases may slightly slow the progression of the disease. Unfortunately, the vulnerability of individuals and families affected by Alzheimer's disease can make them targets for unproven, ineffective, and potentially harmful bogus cures. Such treatments or protocols lack credible scientific evidence, and are intended to prey upon people’s desperation for a solution.
Examples of dietary supplements and so-called natural treatments for which unsubstantiated claims have been made include ginkgo biloba, coconut oil, caprylic acid, omega-3 fatty acids (fish oil), turmeric and curcumin, vitamins E, B, C, and D, ginseng, huperzine A, ashwagandha, lion's mane mushrooms, cannabis and CBD oil, and colloidal silver.
Brain-training apps and games may improve specific cognitive skills. However, there is no good evidence that they can prevent or reverse the underlying pathology of Alzheimer's disease, nor can they provide any meaningful, long-term, overall cognitive benefits.
Beware of lifestyle interventions marketed as cures, such as the Bredesen Protocol™ which requires difficult dietary restrictions and sells expensive proprietary supplements. While a healthy lifestyle is beneficial for overall well-being, there is no convincing evidence to support the claim that any specific diet can reverse Alzheimer's. Dr. Bredesen in particular has been criticized by Alzheimer's organizations for offering false hope based on limited and anecdotal evidence.
It is crucial for both individuals with Alzheimer's disease and their families to base their decisions upon evidence-based medical advice from qualified healthcare professionals. Participating in clinical trials is one way to access new, investigational treatments, while contributing to scientific progress.
The Influence of Diet on Dementia
The complicated relationship between people's diets and their risk of dementia is currently under active investigation. Most diet research is observational, and consequently it cannot demonstrate a cause-and-effect relationship due to the many uncontrolled "confounding" variables. That said, there is a growing body of evidence about what we eat significantly impacting brain health. Potentially, diet can influence the risk of developing dementia and slow its progression.
It is clear that a healthy diet is crucial for overall health, and its benefits likely extend to brain health. A balanced, nutritious, high-fiber diet that's rich in whole fruits, vegetables, grains, legumes, nuts, seeds, and healthy fats, particularly extra-virgin olive oil, may lower dementia risk by half. One such example is the Mediterranean diet, which avoids processed foods, includes a moderate intake of fish, poultry, and dairy, and limits red meat and added sugar. This diet is thought to reduce inflammation and oxidative stress, both of which can contribute to brain damage.
The MIND diet combines elements of the Mediterranean diet and DASH eating plan, emphasizing leafy greens, berries, nuts, olive oil, and fish high in omega-3 fatty acids, while limiting red meat, processed meats such as bacon, ham, and sausages, pastries, and fried foods. Vitamin D3, and B vitamins, especially B12 and folate (B9), may also play protective roles in brain health.
Pre-clinical studies have shown that flavonols have neuroprotective, anti-oxidative, anti-inflammatory, and memory-enhancing properties, based upon their ability to regulate glucose levels, attenuate oxidative stress and inflammation, promote the expression of neurotrophic factors, and regulate signaling pathways. Berries are a mainstay of a flavanol-rich diet, along with onions, kale, lettuce, tomatoes, apples, grapes, tea, and my personal favorites, cocoa and at least 85 percent dark chocolate.
The problem I have with the Mediterranean, MIND, and DASH diets is that they permit alcoholic beverages such as wine and beer. The most current evidence seems to favor the hypothesis that no amount of alcohol is beneficial, and even small amounts could be harmful.
Ultra-processed foods (UPFs), refined carbohydrates such as white bread and pastries, and beverages such as soft drinks that contain added sugar, can produce blood sugar spikes that eventually result in insulin resistance and chronic inflammation, both of which have been linked to increased dementia risk.
UPFs also contain saturated, trans-fats, and modified fats that have been associated with an increased risk of all types of dementia, including Alzheimer's disease. Processed meats such as sausages, ham, and bacon, deli meats preserved with nitrates and nitrites, red meats such as beef and pork, and fried foods, may all contribute to the inflammation that damages blood vessels and brain cells.
These days, most of the meals found in restaurant menus are created for their taste appeal by employing the highly palatable yet unhealthy trinity of sugar, salt, and saturated fats. While essential for the survival of our prehistoric ancestors in an environment of food scarcity, the over-abundance of these three ingredients in modern diets is now killing us, proving the adage that too much of a good thing is a bad thing.
The problem is that our sense of taste has been corrupted by the ultra-processed, mass-produced foods that dominate supermarket shelves and hyper-palatable, fast-food restaurant fare. These faux foods have been engineered for their addictive qualities. They aren't good for us, but they do keep people coming back for me, increasing corporate wealth at the expense of people's health. Fortunately, there are far healthier ways to eat:
Eating healthy foods doesn't have to be boring, but if they taste bland, you may need to rehabilitate your sense of taste. That will help you learn to love eating foods that are actually good for you:
The Fructose Connection
If you've read my book, “Rx for Healthy Eating,” available from Barnes & Noble, the Google Play Bookstore, and Amazon’s Kindle Books, you'll be familiar with the phrase, “Fiber is your friend, fructose is your foe.” My goal has been to encourage people to do more home cooking and prepare easy-to-make meals that are nutritious and delicious, while avoiding highly processed ingredients and limiting consumption of the unhealthy trinity; sugar, salt, and saturated fats.
Emerging research suggests a potential link between high dietary fructose intake and an increased risk of dementia due to Alzheimer's disease. A recently published longitudinal cohort study of community-based older adults who did not have dementia at the time of their enrollment found that those who obtained a higher percentage of their calories from sugar showed a positive statistical association with increased dementia risk.
Among the simple sugars, the monosaccharide fructose, and table sugar, which consists of the disaccharide sucrose (fructose plus glucose) used to sweeten beverages, snacks, desserts, juices, candies, and most breakfast cereals, pose the highest dementia risk, while dextrose (pure glucose) has a lower risk and can be substituted for table sugar in baking recipes.
The term, “type 3 diabetes,” was suggested by pediatric neuroendocrinologist, Dr. Robert Lustig, as a way to underscore a potential link between insulin resistance in the brain and Alzheimer's disease. However, the term is used differently by the American Diabetes Association.
Fructose is mostly metabolized in the liver, unlike glucose, which can be metabolized by most cells in the body. The first step in fructose metabolism bypasses a key regulatory point in glucose metabolism, which leads to excess production of fatty acids and uric acid as metabolic intermediates.
Fat deposits in the liver can interfere with insulin signaling pathways by decreasing the expression of insulin receptors. Elevated uric acid levels in the blood have been associated with insulin resistance and metabolic dysfunction in a recent meta-analysis.
A proposed mechanism for the relationship between fructose and dementia involves higher blood levels of insulin reaching the brain due to insulin resistance. The same brain enzyme that deactivates insulin also breaks down amyloid proteins. Higher insulin levels compete with the amyloid's metabolism, so less of it gets broken down, resulting in amyloid plaque deposits. While this explanation may be overly simplistic, the metabolic changes that occur in diabetes do appear to accelerate the progression of Alzheimer’s disease.
Glucose metabolism in the brain is necessary for energy production and healthy cognitive functioning. Its metabolic pathway involves adenosine triphosphate (ATP) production, the primary intracellular energy source. High fructose intake, linked to insulin resistance, may also lead to a depletion of ATP in the brain, and this energy deficit can impair normal brain function. Impaired glucose metabolism in the brain is a characteristic feature of Alzheimer's disease, often preceding the formation of amyloid plaques and tau tangles, as detailed in a 2016 review article.
Fructose overconsumption also contributes to obesity, dyslipidemias, and chronic inflammation. Its metabolic byproducts play a role in several metabolic diseases, and can impair brain function, according to a 2020 animal study. Other studies have shown that long-term fructose administration can lead to the accumulation of amyloid beta and tau proteins in the brain, hallmarks of Alzheimer's disease.
The breakdown of fructose produces uric acid. When uric acid is elevated in the brain, it can contribute to inflammation, which is a key factor in neurodegeneration, according to a 2024 review. Fructose metabolism can also increase oxidative stress through an imbalance between free radicals and antioxidants, which also damage brain cells.
The high-fructose corn syrup and added sugars in processed foods and sweetened beverages rapidly deliver large amounts of fructose to the liver, resulting in the formation of toxic metabolites. In contrast, the amount of fructose contained in whole, fresh fruits, are accompanied by fiber and other beneficial compounds, and don't have the same toxic effects because of its slower absorption. Eating fruit along with protein also slows down fructose absorption and enables the liver to keep up with its detoxification.
The toxicology maxim, “The dose makes the poison,” is particularly true when it comes to fructose. The damage done by this especially sweet of poison is mitigated when smaller doses are absorbed over longer periods of time. While the evidence linking fructose and dementia continues to grow, more human studies are needed to fully understand the nature and extent of this relationship. In the meanwhile, limiting added sugars and avoiding high-fructose corn syrup are prudent strategies for optimizing our overall brain health.
Institutional Living and the Healthy Eating Challenge
The “memory care” unit now housing my loved one is located in one of the nicer assisted living facilities in our area. Its euphemistic name is intended to conceal the fact that it is actually a locked ward, and its inmates are not free to come and go as they please. Its function is to provide a safe environment in which they can live out the remaining days of their terminal illness.
I had high expectations for the quality of care and feeding that its residents would receive, and was disappointed to find that the meals are not “home cooked.” Instead of being made from scratch using an in-house selection of healthy ingredients, they are provided by a restaurant food service.
Although this particular service claims to support healthier menus, and says that they have the ability to offer a selection of fresh produce and plant-based dietary alternatives (presumably at a higher cost to the institution), the meals I’ve seen served to the residents, as is typical with most restaurant fare, prioritize taste over nutrition. Along with smoking, drinking, and the absence of exercise, I refer to unhealthy diets as “installment-plan suicide.”
From what I've observed, the food service meals, while providing adequate amounts of protein, are typically low in fiber and high in added sugars and refined carbohydrates. As the facility's nurse explained to me, “We don't want our residents to lose weight when they don’t eat enough.” However, this kind of “diabetogenic diet” will produce rapid spikes in blood glucose levels, straining the ability of the pancreas to produce enough insulin. Over time, it can lead to insulin resistance, and eventually type 2 diabetes.
Fortunately, I’ve been able to negotiate a diet plan for my loved one that avoids most refined carbohydrates and saturated fats, and increases the amount of fresh, whole fruits and vegetables served at each meal. The staff now has orders to not offer her calorie-laden desserts and snacks, since she has trouble remembering that she doesn’t eat such things and might take them just to be polite.
The Influence of Exercise on Dementia
Avoiding frailty due to sarcopenia is of vital importance for seniors. This demographic requires an increased intake of protein, along with a commitment to daily resistance exercises, in order to maintain their muscle mass. When calories from carbs compete with protein consumption, and regular exercise is neglected, that's a recipe for sarcopenic obesity.
Staying active throughout one's life may help protect against cognitive decline, even when the key markers of Alzheimer's disease are present, according to a new study. Researchers found that regular exercise, especially before the age of 50, can preserve brain volume, particularly in those areas that are linked to memory and thinking. The prospective observational study tracked 5,362 people, and the data suggests that exercising throughout life is associated with better cognitive functioning at age 70.
According to the researchers, “The evidence shows that it's never too early or late to start making positive changes.” People who reported exercising once or more a month before the age of 50 tended to have less shrinkage in the hippocampus, a part of the brain involved in learning and memory. The benefits of exercise were even more pronounced in women.
Institutional Living and the Daily Exercise Challenge
Residents in the assisted living section of the facility have access to an exercise room, with equipment and classes suitable for seniors, but the memory care unit does not. I’ve persuaded the memory care staff to escort my loved one to the daily exercise classes, and have placed some exercise equipment in her room.
A 2025 systematic review of research found that engagement in physical exercises and leisure activities that include cognitive challenges were the most important modifiable factors for lowering the risk for stroke, dementia, and late-life depression. The analysis pointed to interconnections between increasing physical activity and better blood pressure control, improved sleep and eating habits, and more social interactions, all of which are beneficial.
Having to deal with the care and feeding of a person with Alzheimer's disease has been very challenging, and is providing me with a very intense learning experience. In the past, my patient population included some who had major psychotic disorders, but I had neither understanding nor qualifications for helping patients with dementia.
Alzheimer’s is an illness that we’d rather ignore, but developing dementia ourselves is something that we might someday need to face. Support for the basic research necessary for the development of effective treatments is essential, and it has been crippled by the Trump administration’s assault on science and conventional medicine.
It is time for all of us to recognize that dementia is a serious public health problem. The prevalence of Alzheimer’s disease is increasing as the population ages, but it’s not simply a matter of people living longer. Its rise reflects a convergence of aging demographics, chronic diseases such as obesity, type 2 diabetes, and hypertension, environmental risk factors such as air pollution and toxic chemicals, and earlier diagnosis.
At the same time, unhealthy modern lifestyles include: diets deficient in nutrients; high-calorie and ultra-processed foods; sedentary behavior; inadequate sleep; social isolation; and psycho-social stressors. These all contribute to dementia risk, as well as other chronic conditions. You might want to reconsider your own lifestyle, and take steps now to ensure that it adequately addresses the modifiable risk factors that have been identified for this devastating disease.
Daily Fluctuations in Alzheimer's Symptoms
One of the common frustrations for caregivers is the day-to-day variability in Alzheimer's symptoms. You never know if your loved one will seem better or worse on any given day. Daily fluctuations generally tend to become more pronounced as the disease progresses. Symptom variability can result from several interconnected factors:
Physiological Factors
Circadian rhythms can influence cognitive functions, and many people with Alzheimer's disease experience the phenomenon known as “sundowning.” They have increased confusion, agitation and behavioral issues that occur in the late afternoon and evening.
Poor sleep quality for one night often leads to worse symptoms the following day.
If the person is taking medications, fluctuating drug levels in their bloodstream can have an effect on cognition and behavior.
Even minor infections, such as an otherwise asymptomatic UTI (urinary tract infection) can dramatically worsen cognitive symptoms.
Both blood sugar and hydration levels can significantly impact cognitive function.
Environmental Factors
Novel environments and unfamiliar surroundings often increase confusion.
Sensory stimulation levels can play a role, with both over-stimulation and under-stimulation causing symptoms to worsen.
Disruptions of established routines often trigger symptom increases.
Psychological and Emotional Factors
Anxiety, stress, or excitement can worsen cognitive symptoms.
Mental exertion earlier in the day can cause fatigue and deplete cognitive reserves.
The “Good Days” phenomenon can present with no known cause. People with Alzheimer's disease sometimes experience temporary periods of improved clarity, while the underlying pathology (amyloid plaques and tau tangles) remains relatively stable day-to-day.
For more information about preventive medicine and brain health, see:
― ― ―
This Post can be updated at any time. Please check back here again to find the most up-to-date information.
You can find many more articles about Healthy Living in my Post Archive.
Please share my Website Link with others via your social media accounts. You can help your friends and followers become healthier by suggesting that they subscribe to my totally free Newsletter.